Optipedia • SPIE Press books opened for your reference.
Ophthalmoscopy
Excerpt from Field Guide to Visual and Ophthalmic Optics
Viewing the retina and optic disc is useful for diagnosing diabetic retinopathy and observing the deleterious effects of glaucoma. Common methods for viewing the retina are direct and indirect ophthalmoscopy. A direct ophthalmoscope is a small handheld device in which light is directed into the eye of a patient. Light emerging from the eye passes through a lens and into the observer’s eye. The lens power is adjusted to image the patient’s far point to the observer’s far point. Typically, the observer is limited to a 10° patch on the patient’s retina. This technique is useful for viewing cupping of the optic disc from elevated intraocular pressure. Swelling (edema) and hemorrhages can also be seen.
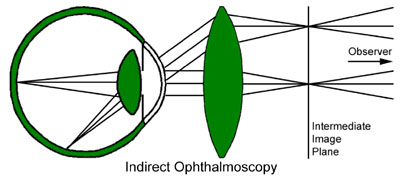
Indirect ophthalmoscopy uses a head-mounted illumination system and a large aspheric lens. The lens is held at arm’s length in front of the patient’s eye. Illumination on the observer’s head passes through the lens and enters the eye. Light exiting the eye passes through the lens and forms an intermediate image between the lens and the observer. The headgear may also optically increase the stereo angle between the eyes of the observer to exaggerate the three-dimensional structure of the retina. Indirect lenses are usually single aspheric elements. Back reflections from the surfaces are problematic, so single elements reduce the number of surfaces to reflect light. Anti-reflection coatings are valuable at reducing this difficulty. The asphericity of these lenses is designed to minimize distortion. Much larger fields of view can be obtained with this method.
J. Schwiegerling, Field Guide to Visual and Ophthalmic Optics, SPIE Press, Bellingham, WA (2004).
View SPIE terms of use.