Device standards bring a new light to clinical imaging
Photoacoustic devices are bringing new light to clinical imaging. Photoacoustic imaging (PA), also known as optoacoustic imaging (OA), uses one or more laser wavelengths tuned to specific biological features to, in turn, induce ultrasonic waves in tissue. This imaging modality has been explored in research and pre-clinical settings since the 1990s and is approved for clinical use by the US Food and Drug Administration and its European counterparts.
The advent of a new imaging modality is a diagnostic game-changer, and the broad adoption of new technology requires a clear path for integration into the clinical workflow. The development of PA standards compatible with Integrating the Healthcare Enterprise (IHE)—an industry effort to improve how computer systems in healthcare share information—establishes the pathway for this new modality to become a tool in the clinical imaging portfolio. As a first step, the PA clinical image format and imaging metadata were standardized via DICOM (Digital Imaging and Communications in Medicine), the international standard for medical images and related information.
Standardization for PA was first promoted in 2018 through the International Photoacoustics Standardization Consortium (IPASC). The consortium codified parameters relevant to PA research and development. As PA matured towards clinical adoption, formatting the technology’s output data to complement existing imaging workflows became a driving need.
IHE-scheduled workflow is the medical imaging community’s accepted interoperability profile. DICOM requires the acquisition modality to transmit images to an image archive. Conformance to DICOM standards enables a high level of equipment compatibility at every medical imaging facility.
As PA data representation needs are different from other imaging modalities, in 2020, a new DICOM working group (WG 34) for PA was established. It is a consortium of imaging vendors and users, supported by SPIE, tasked with developing a clinical DICOM Photoacoustic Imaging Information Object Definition (IOD).
How that IOD is crafted requires deep knowledge of the DICOM standard along with an understanding of how it is expected to interact with other DICOM services or IODs. Hammering out an optimized data object required balancing the goals of the PA community with the guidelines of the DICOM framework. The process provided working-group members with many opportunities to learn, test, and be mentored by others in the DICOM community.
The working group followed DICOM’s rigorous supplement process to create the PA IOD. A DICOM supplement begins with the working group submitting a new work item proposal to the DICOM Standard Committee. Once a supplement is approved, a series of versions are created and presented to DICOM Working Group 6 (WG 6). The first read allowed WG 6 to provide WG 34 feedback on its direction and information on items that need to be addressed. Along the way, the PA working group members met with other DICOM working groups and subject matter experts to resolve issues.
The process—which ultimately took two-and-a-half years to complete—also involved steps for public comment and letter ballot versions to be presented, generating comments that required resolutions and secondary review before a final text version was approved and released in DICOM standard 2023c.
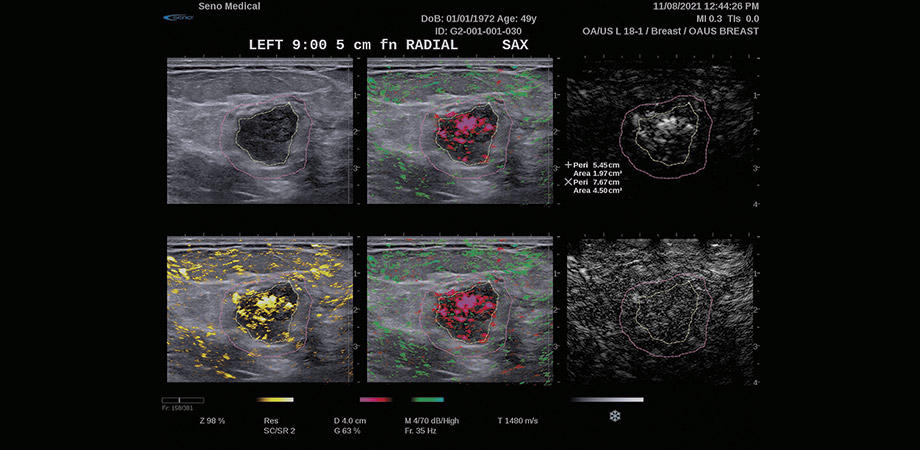
During the development of the DICOM PA IOD, the working group had to identify the core set of information common to all PA systems (metadata and image data). PA equipment geometries include handheld scanning, tomography, and microscopy. Applications are similarly diverse, including dermatologic imaging and breast cancer imaging and diagnosis. The PA DICOM IOD needed to provide the elements these imaging systems share (e.g., laser settings, light transmission factors) while allowing the flexibility to represent different clinical scenarios.
Finding a flexible format for storing many kinds of PA data was challenging. Most DICOM IODs divide 2D and 3D images into different formats, either supporting 2D images (single or multi-frame) or 3D images, but not both. Some current PA systems have been coupled with conventional ultrasound systems that generate 2D image frames over time as the transducer is scanned. Three- dimensional PA data is also of interest for support of PA tomography and for handheld PA 3D scanning systems. Before there was a recognized PA DICOM IOD, existing manufacturer implementations used workarounds such as encoding data with custom image formats or burning in PA data to the coupled modality images (for example, ultrasound).
In looking for a DICOM pattern that would help cover the breadth of the PA field, the “enhanced class” of DICOM imaging IODs was found to be a good model to provide flexibility. Manufacturers can tailor their data representations by flagging dimensions of the temporal position time offset and image position (volume) on each acquired data frame, thus allowing a device to indicate whether image frames were acquired as 2D slices over time (e.g., handheld scanning) or as a volume of data considered to have been acquired at one time (e.g., tomography). A third dimension, the image data type sequence, is applied to each acquired image to define the photoacoustic imaged property (clinical characteristic) for each image. This is important because a single clinical acquisition may result in multiple images, each containing the response to one or more laser wavelengths.
A constrained set of metadata parameters will help standardize imaging information from different manufacturers. WG 34 sought areas where common concepts could be identified. Several new DICOM concept identifier (CID) tables were defined with coded values representing parameters of PA. One common concept identified in a new DICOM table was the PA imaged property, the clinical characteristic being imaged (blood oxygenation level, hemoglobin, elasticity, perfusion, melanin, water, or lipid). Other common concepts identified in new DICOM tables contribute to the image reconstruction: PA illumination method, acoustic coupling medium, transducer technology, speed of sound correction mechanisms and PA reconstruction algorithm family. Additional values are anticipated for the CID tables as more PA applications are brought to market.
The addition of PA to the DICOM 2023c standard was a great accomplishment for the community, although much remains to be done to ensure that the standard becomes a fully integrated part of the clinical workflow. As a community, we need to continue to create datasets for image archives and viewing applications to drive PA adoption. WG 34 also has interest in defining fusion details to support more dynamic clinical representations of PA with coupled modality images or to allow selection of the response of one or more PA wavelengths for display. Finally, as its core mission, WG-34 will continue to adapt and grow the DICOM standard as PA imaging technology evolves.
Allison Bertrand is co-chair of DICOM Working Group 34 and director of software interoperability at Seno Medical Instruments.
Brian Bialecki is co-chair of DICOM Working Group 34 and director of IT standards and interoperability at the American College of Radiology.



